The transcript from the FDA’s recent public workshop on Patient Focused Drug Development (PFDD) makes interesting reading. The workshop was held in December as part of the FDA’s commitment to develop four guidance documents on obtaining meaningful patient input that can inform regulatory decision-making. Last month’s workshop focused on Guidance 1 which is about collecting comprehensive patient community input on burden of disease and current therapy.
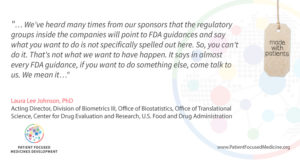
Speaking at the workshop, FDA’s Dr Laura Lee Johnson said:
What does this mean for those committed to patient engagement (PE) who face barriers from legal, compliance or similar departments within their organisation? It means that lack of specific FDA guidance cannot be cited as a reason to not do PE – it means there is one less ‘excuse’ for not implementing PE efforts. It means that if you have a potentially promising PE approach or initiative but are not sure whether it is permissible, you can reach out to FDA on a case by case basis and ask for advice.
Dr Johnson goes on to say that this is an ‘evolving field’ – that’s exactly true and exactly why it would be impossible to expect guidance that is so comprehensive it covers every potential need. It’s impossible because we are still in the infancy of PE in many ways – we are all still learning and doing and learning again so there are no hard and fast rules yet, only concerted attempts to do better. Doing better means sharing and learning from experience, and collaborating in pre-competitive multi-stakeholder alliances to co-create solutions to common challenges. This is why PFMD was established – to bring together and synergise the PE efforts underway so we can collectively and more efficiently move the needle in PE.
Guidance 1 from the FDA will provide a ‘framework for collecting representative patient input that can be used to inform clinical outcome assessments, patient preference information and a whole host of other types of research’. In other words, Guidance 1 is about who you ask for input, why you have chosen this group and how you get their input. During the meeting, Guidance 2 was described as understanding what to ask and why – developing a list of impacts that are important to patients. Guidance 3 is deciding what to measure in a clinical trial by prioritising that list to what is actually measurable, and Guidance 4 is about selecting the right endpoints and associated tools for the trial that are ‘considered significantly robust for regulatory decision making’.
The FDA workshops are delivering real tools and practical outputs that can be used to implement more meaningful and effective PE. The Guidance documents – and opportunities to help shape these – are eagerly awaited.
Patient engagement? No more excuses…
Tags:

































































