Danielle Barron speaks to PFMD co-founder Tony Hoos about his recent participation at the EFGCP Annual Conference in Brussels
What is an acceptable level of uncertainty? What is an acceptable benefit/risk ratio? These questions and many others were asked during the European Forum of Good Clinical Practice 2019 annual conference. Held in Brussels in late February, the meeting sought to answer these questions within the context of clinical trials and novel R&D strategies, as well as exploring patient-driven initiatives for a roadmap to health.
PFMD co-founder Tony Hoos delivered the kick-off presentation of the day dedicated to patient involvement, entitled “Patients are an integral part of R&D in Healthcare – What is their role overall and in protocol development and execution?”
Hoos first asked his audience to consider the many different types of patients, and how their needs and wants can vary considerably.
“There are different types of patients – think of a child who needs to be vaccinated or an adult with cancer or someone who is traumatised after an accident. One cookie-cutter solution does not fit all.”
According to Hoos, the key questions for everything in drug development boil down to: What’s an acceptable level of uncertainty, and what’s an acceptable level of benefit/risk?
“That translates into how much knowledge do you need in order to make a drug available. If you know everything then there is no uncertainty, but it may have taken way too many years to make a drug available. As for the acceptable level of benefit/risk, that depends on the stakeholders and their situation. As a patient, for example, if you are very sick, you might accept a very high risk for some benefit, but when you are super healthy and need a vaccine, you would probably say the risk is low so I want a high benefit,” he explained, adding that there are different levels of tolerance among healthcare providers, regulators and payers.
Hoos also took the opportunity to highlight the fragmented nature of patient involvement in drug development, saying that historically stakeholders often acted in “functional and geographic isolation”; this led to suboptimal outcomes for patients and societies as well as high cost.
“The regulators have done their thing and so have the payers. Industry has done its thing, and few patient groups have worked with all stakeholders. At present we have almost a perfect storm because the current way the healthcare systems operate is unsustainable. There are huge cost pressures. Drug development is too expensive. Any changes to drug development driven by what an acceptable level of uncertainty is and what benefit/risk ratio can be accepted must be agreed by all stakeholders. As an example: there is no point in industry shortening a clinical trial by eliminating a placebo arm if the regulators or payers do not accept it.”
Patient-centric models of healthcare and multi-stakeholder alignment is what is needed, he says. “Patients need to be involved from the early stages of research right through until the product hits the market and not just in one trial.”
Drug development involves central questions that require patient involvement, says Hoos; for example, is the clinical development program/trial acceptable from a patient perspective? Patients should be involved in the design, execution and interpretation of trials. This will lead to improved execution and improved relevance to them and all other stakeholders, i.e. faster and more economical access to medicines. Yet the current clinical trial process does not involve patients in all of these questions, he says.
Also discussed was recent research regarding patient involvement in clinical trials
A recent study by The Economist Intelligence Unit, published in December 2018, found that recent innovations in clinical research, such as adaptive design trials, patient-centric trials, precision medicines, and real-world data trials create the real return. The effect and impact of patient-centric was shown to be huge.
“The Economist study found that patient-centric trials increase the odds of a product making it to launch by 20%. It also shows that the recruitment time is accelerated by several months. That is a huge benefit for everybody,” notes Hoos, adding that this finding backs up what has been shown in previous studies.
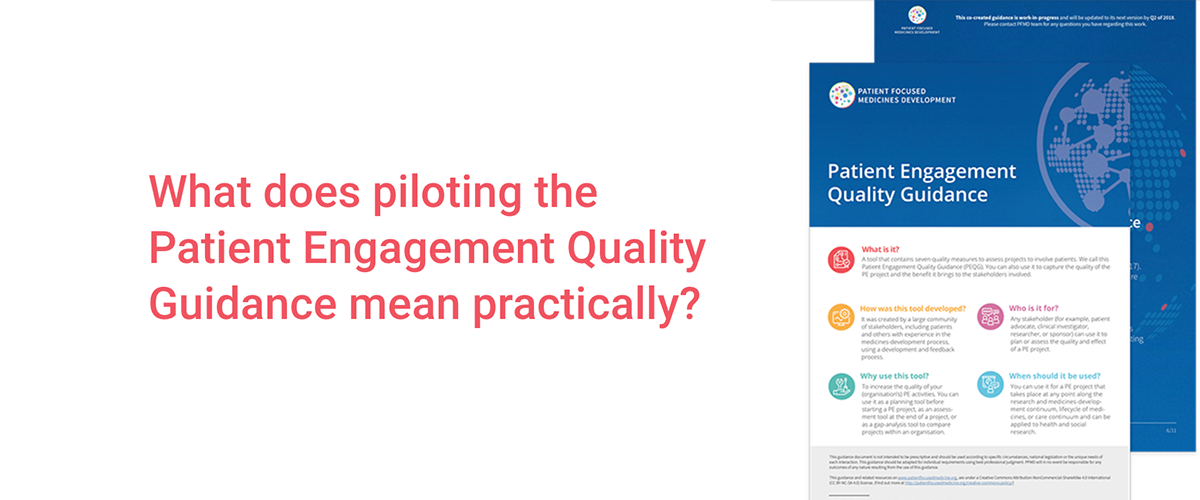
The PFMD co-founder also took the time to discuss the endeavours that PFMD has been making since its inception, highlighting the PE Quality Guidance, Synapse and Book of Good Practices, among others.
He concluded his presentation by reiterating there is no “one-size-fits-all” process, but agreement on standards and impact of patient involvement is key, and re-stating that patient-centric trials are needed.
It is Hoos’ belief that the system will only change if all stakeholders come to the conclusion that patient involvement in drug development is of real benefit and they agree on how to do it.
“Patient involvement in clinical trials leads to real enhancement of the development, increases the likelihood of success for launch, and decrease the time of development. People are beginning to realise that if they don’t talk to patients they may have a lower NPV – the disadvantages of not involving patients are becoming clearer, so it is making people more motivated to do so.”
Different patients, different solutions: PFMD at the EFGCP Annual Meeting
Tags: