Big data has big potential to change healthcare. But, if patients are to buy into this vision of the future – and share their data – the benefits to their care must be made clear
The capacity of digital tools to improve health and deliver value to all healthcare stakeholders is a hot topic. Health systems and payers hope care can become more efficient while improving outcomes; health professionals see opportunities to apply their skills where they can do the most good; while patients see a pathway to more convenient care and, ultimately, improved quality of life.
While the interests of these groups may overlap, they are not the same. And, as patient data is the fuel required to power the digitized healthcare future, it is essential that the needs of patients – and the outcomes that matter to them – are central to the brave new world that is emerging. In addition, it will be vital that patient privacy, data security and information ownership are paramount to discussions about how healthcare evolves.
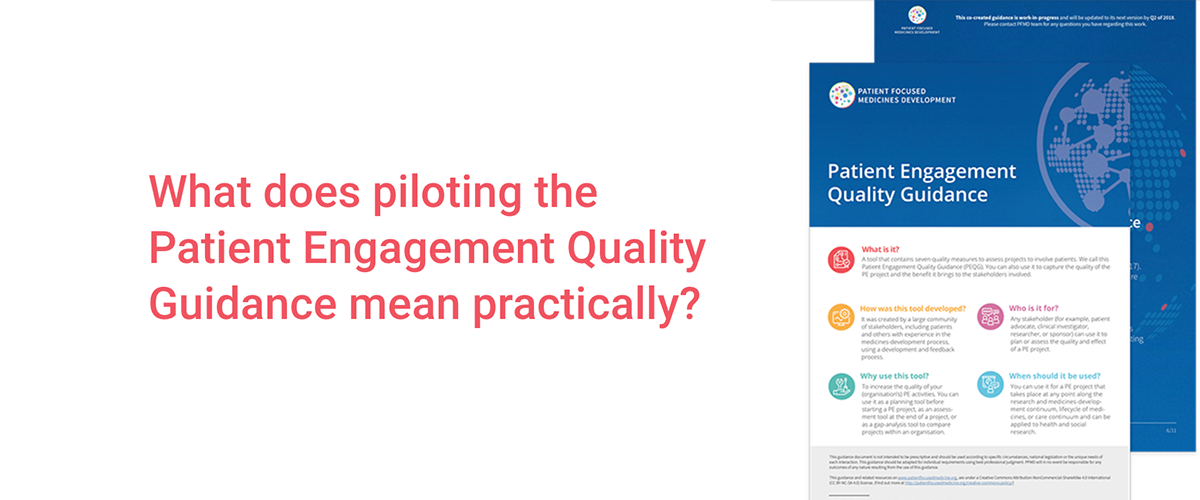
These were among the themes discussed at a virtual session of Patient Engagement Open Forum (PEOF) on June 24. A range of experts, including patients, explored the potential of data to advance healthcare and the need to involve patients in building a trustworthy data ecosystem. The event built on an April 2021 session of the PEOF which had addressed the role patients can play in the fast-moving world of digital health.
Bridging the gap
Introducing the interactive webinar, Nicholas Brooke, PFMD Executive Director at The Synergist, highlighted the gap between the potential of digital and the reality of how patient-shared data is currently used. ‘This is a real trust breaker,’ he said. ‘We must change how data is managed. Patients and patient organisations could play a role in unlocking the full potential of patient data if trust can be built.’
Open science offers a way forward that would prioritise the greater good by offering all stakeholders the benefits of access to data, according to Névine Zariffa, Principal and Founder, NMD Group. When COVID-19 struck, Zariffa saw an opportunity to jump-start innovation. She launched the International COVID-19 Data Alliance (ICODA) to provide a platform for sharing scientific data on a global scale.
‘There are thousands of trials underway looking at COVID treatments,’ Zariffa told the meeting. ‘Our goal was to bring together summary-level data from multiple trials to enable researchers to generate new insights into COVID-19 treatments. This would provide a way to investigate sub-populations and secondary endpoints which are usually under-represented or under-powered in individual trials.’
The not-for-profit initiative attracted 10 pharmaceutical companies and collated several datasets but has yet to achieve its vision at scale. ‘People who provide data tend to see the downside to sharing while those who use data only see the upside. There’s a gap – the incentives are not aligned.’
She called on investigators to ‘enable onward use of data’ after their primary research is completed, and for funders and policymakers to require openness from scientists: ‘If you’re conducting a trial, your job is not done until you’ve shared the data from that trial.’
Outcomes that matter to patients: quality of life
While research on COVID-19 and other infectious diseases usually looks at interventions that can reduce the acute effects of illness and improve survival rates, a growing proportion of trials now look at long-term illnesses such as diabetes. This requires disease-specific outcome metrics that are best developed with patient input.
‘The majority of diseases are chronic diseases,’ explained Dr Matthias Rose, Professor and Chair of the Department of Psychosomatic Medicine at the Charité – Universitätsmedizin Berlin. ‘For these patients, the outcome is health rather than survival which may have been the top priority 100 years ago. Today, we cannot define health from a disease perspective; it has to be from a patient perspective.’
To achieve this, a structured, standardised way to assess patients’ health is required. This should prioritise increasing healthy life years and delivering what matters to patients rather than the clinical metrics that are the focus of healthcare providers.
Dr Rose is working on the H2O project – a major public-private initiative co-funded by the EU and the pharmaceutical industry – which aims to collect standardised health data in an ethical and socially responsible way.
https://www.youtube.com/watch?time_continue=8&v=oGadCf52nfE
At the heart of H2O will be the creation of Health Outcome Observatories that collect integrated outcomes (clinical outcomes and Patient Reported Outcome Measures (PROMS)). To begin with, four national observatories will be established in Austria, Germany, the Netherlands and Spain, with an overarching European hub. These will focus initially on diabetes, inflammatory bowel disease and cancer. If successful, expansion to other disease areas along with the addition of hubs in the UK, Belgium, Sweden, Italy and Denmark.
Ultimately, the project could empower patients with digital tools that they would use to manage their health and report outcomes while retaining control of their data. By pooling integrated outcomes, the observatories would generate meaningful insights which could inform healthcare decisions and improve outcomes for all.
‘This is the first attempt to do this at scale in Europe,’ said Tom Metcalfe, Data Policy Leader, Personalised Healthcare at F. Hoffmann La Roche. ‘H2O aims to make data available to clinicians and patients at the point of care, and to support the work of other interested parties including innovators, regulators, HTA agencies and patient organizations.’
Informing two-way conversations
H2O is committed to integrating patients and patient representatives into all aspects of the project. Responding to the presentation, Jan Geissler, founder and managing director of Patvocates, welcomed this aspiration and expressed his hope to see it translated into substance as the initiative gets off the ground next year.
‘We often see decision-support systems being built to support physicians during consultations,’ he said. ‘The goal must be to have a two-faced system that gives both parties – clinicians and patients – data so that they come to the conversation with relevant information.
Looking at the broader task ahead in unlocking the potential of healthcare data, Geissler said data-sharing models should serve the interests of patients, particularly if patients are asked to share some of their data for the greater good. Stakeholders need to think at the design stage about how data-driven systems can help the patient community. If this is done well, patients are more likely to help researchers to access the right data.
The event concluded with an interactive “GroupMap” exercise that allowed participants to brainstorm ways to improve the use of data in healthcare. This helped to highlight some of the challenges that lie ahead, along with constructive ideas on how to accelerate progress in a field buzzing with potential.
Do not forget to join us at the Patient Engagement Open Forum, register now for the October 2021 sessions.