The article is written by Dr Katherine Deane and edited by Ifeanyi Sargeant (Editorial Coordinator, Patients Focused Medicine Development)
Dr Katherine Deane (Senior Lecturer in Research, School of Health Sciences, University of East Anglia, UK), talks about the importance of getting diverse patient populations involved in designing and participating in trials and how PFMD’s Patient Engagement Quality Guidance can help.
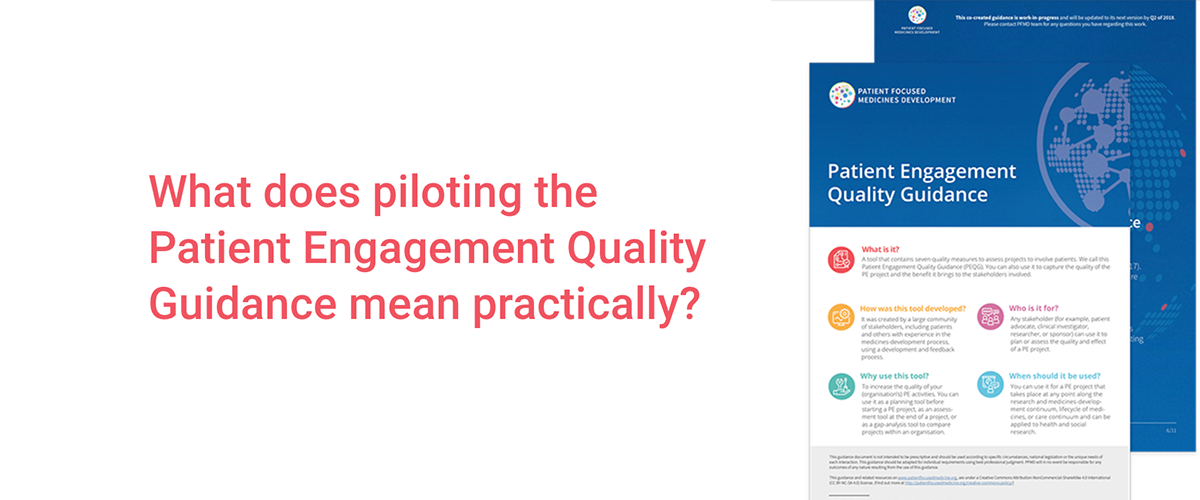
I recently presented PFMD’s Patient Engagement Quality Guidance at Parkinson’s UK Research Conference. What struck me was the number of people in the room taking notes. I had assumed that the things I was saying were obvious but the audience response said otherwise. As someone who uses a wheelchair, I live it every day and there are things I think about all the time – transport, accessibility, parking nearby, length of meetings, paperwork requirements… The list is long which means that becoming an involved patient can be challenging. Putting in place processes and conditions that take into account the needs of the patients you want to get involved is key to the success of any patient engagement initiative.
If you work ‘normally’ without tailoring for patient involvement, you will exclude many of the people you want to include but you won’t know why. Patients will simply not show up – not because they don’t want to, but because they can’t (for logistical or other reasons). Unfortunately, their non-appearance can be misconstrued as lack of interest. This lack of engagement can have long-reaching consequences. For example, not implementing conditions for patients to get involved in the design of a clinical trial means that the trial will be set up with inherent barriers that will exclude key populations e.g. those with additional access needs. It also means that the data from these trials will not represent the population intended for the intervention. If minority groups – including people with disabilities, comorbidities, or older patients – are unable to take part in studies, the trial results and treatment decisions based on them will be skewed, unrepresentative and potentially misleading. There needs to be a paradigm shift in thinking to understand that the problem that needs to be overcome is the system and processes not the disability or other issues that exclude different groups. We need to take a step back and look at our unconscious biases and challenge them at all levels so research works for everybody.
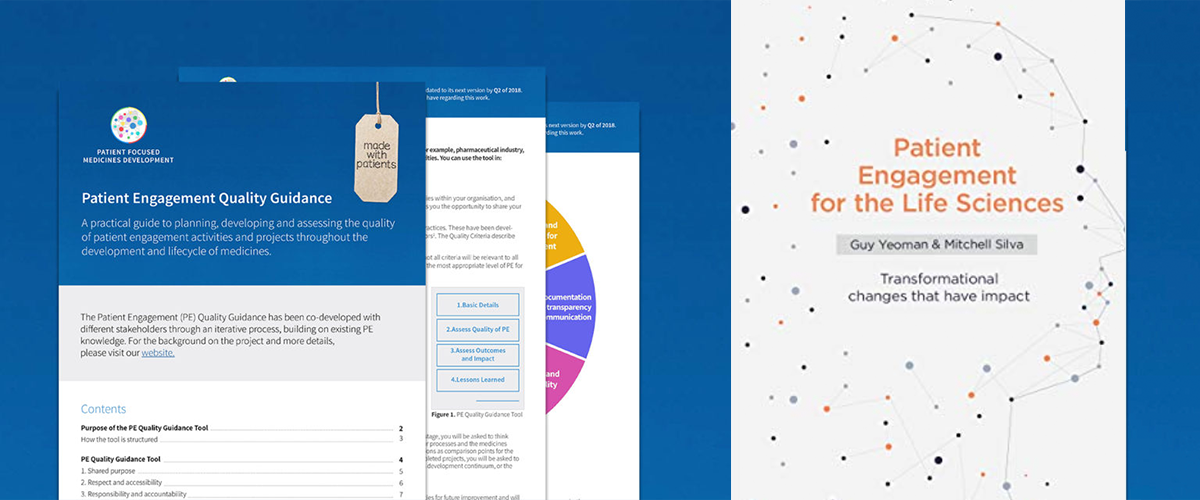
The climate of patient engagement is changing – we have moved from ‘should we’, to ‘HOW should we’. This is why PFMD’s Patient Engagement Quality Guidance is so valuable. It provides the HOW with concrete and actionable advice to help anyone wanting to do better patient engagement. The granularity within the Guidance is particularly important and has been generally lacking. For example, a researcher wanting to get patient advice through a face-to-face meeting can use the Guidance and it’s ‘Have you thought about…?’ approach to identify potential barriers to patient participation (such as timing, building access, meeting length) and organise the meeting appropriately to remove these. These often overlooked, practical issues can prevent patient engagement activities from being successful.
Presenting the Patient Engagement Quality Guidance at the Parkinson’s UK conference was timely for several reasons. Firstly, Parkinson’s UK were one of the early members of PFMD and have been involved in co-creating the Quality Guidance so it was a great opportunity to share the outputs and feedback. Secondly, Parkinson’s UK launched new Patient and Public Involvement (PPI) Guidance for researchers at the conference which complements the Patient Engagement Quality Guidance. There was also a workshop at the conference aiming to raise the visibility of patient engagement so that it is not an optional add-on but an intrinsic and accepted part of research methodology and presented as such. Patients need to be part of the steering group, informing the research targets, the outcomes measures, the design of the process, not just providing data as participants in the research.
We live in an exciting era for research with innovative therapies emerging. However, these therapies will only be valuable for patients if they address the issues that matter most to them – the issues they are struggling with. In many cases, cutting-edge science solutions are not the answer – managing more practical aspects (such as urinary incontinence, depression and anxiety), that have a massive impact on quality of life may be the patient’s priority. Only by ensuring meaningful patient engagement can we identify and focus on patient priorities.
Our hope is that sharing the Patient Engagement Quality Guidance will encourage its uptake and implementation to build the evidence-base for what ‘good’ patient engagement looks like. As a result of the presentation, I was invited to attend a National Institute for Health Research (NIHR) event which provides a new opportunity for further dissemination and to connect more patient engagement networks.
The climate of patient engagement is changing from ‘should we’, to ‘how should we’
Tags: